Testimonials
Bill T. - Triple Bypass
Every February, Bill T., a 57-year-old television freelancer who covers sporting events, heads to Florida for Boston Red Sox’s spring training. A typical day for him begins with a three-mile walk with his wife. On one particular morning walk in 2018, Bill felt a pain in his chest that would come and go. He chalked it up to acid reflux caused by his hiatal hernia.
When the Mansfield, Massachusetts native returned home, he followed up with his cardiologist. Bill had a stress test and EKG, which both came back normal.
“After I met with my cardiologist, I went on acid reflux medicine for several months,” explains Bill. “But the pain was getting worse, and I knew it wasn’t acid reflux as the pain was going into my back. Also, it would only happen when I did physical activities, specifically exercises using my legs, such as lifting weights or walking.”
As time went on, Bill found he got winded when hauling his TV equipment, and it got so bad that he could only walk a short distance and then would need to stop to catch his breath. A final episode, which took place at Gillette Stadium while he was covering the final New England Patriots’ football game of the season, landed him back at his cardiologist’s office.
“I knew something was wrong and told my cardiologist it wasn’t my hiatal hernia acting up,” he says. “The doctor ordered a CT scan with dye, which found my widow maker artery clogged 90 percent and two other blocked arteries.”
Now with a diagnosis, Bill’s doctor gave him many options to review and consider as to where to go for further treatment.
“My extended family wanted me to go to another Boston hospital that they were more familiar with, but my cardiologist strongly recommended Dr. Agnihotri and St. Elizabeth’s and I’m so glad he did,” explains Bill. “It was the way he spoke of St. Elizabeth’s that sealed the deal for me.”
Dr. Arvind Agnihotri, who is the chief of the Steward Center for Advanced Cardiac Surgery and leader in the field of cardiac surgery, performed Bill’s triple bypass procedure on December 17, 2018.
“Leading up to the procedure I was scared about having open heart surgery,” says Bill. “But every single staff member at St. Elizabeth’s was outstanding. They kept reassuring me that they deal with this all the time and that I was in good shape, mainly because I didn’t smoke.”
On the night before the surgery, one specific nurse, Fran, who also had a great sense of humor, helped Bill relax by telling him he was going to do great the next day. “Fran and all of the staff explained what was going to happen, every step of the way. It was nice to know everything, and it prepared me for what was going to happen next,” he says.
“After the surgery, I was surprised to find myself not minding being in the hospital. My room at St. Elizabeth’s felt like a hotel room – it was bright and cheery. I felt relaxed and could sleep,” says Bill. “My wife and I were so impressed with everyone who cared for me, from the health care team to the cleaning people to the people who brought my meals.” Bill’s recovery from the open bypass surgery went very well. He now walks every day with his wife by his side and is happy to be back golfing, fishing and kayaking. And, even though he missed some of spring training, he was back at Fenway Park for the opening games.
“I couldn’t believe it. I was able to pull my cart with equipment weighing 300 pounds throughout Fenway Park, and for the first time in a year I didn’t have to stop, and I didn’t get winded,” he says. “I am so grateful for Dr. Agnihotri and his team for getting me back into the game.”
A Dancer's Comeback
As a multi-hyphenate professional ballerina-radio personality-stand-up comedienne, Carolyn P. from Hartford, Connecticut poured much of her boundless energy and her heart and soul into her first love as a dancer. As the principal dancer, director and choreographer with CONNetic Dance, Carolyn was looking forward to the debut of “Nutcracker Suite & Spicy” that she was instrumental in bringing to the stage.
However, in December 2017, right before the opening, that all changed after a freak fall on ice that left her with a traumatic ankle injury.
As a classically trained ballerina, Carolyn has had her fair share of minor injuries but never anything significant. “I’ve had minor injuries and aches and pains in the past and have been able to push through them and continue dancing,” said Carolyn. “This time, I fell and heard a noise and immediately knew that I had broken something. I wanted to see, and I took off my boot and I will never be able to un-see it as my foot was almost backward. It was a very graphic injury. I very quickly felt dread, particularly as someone who relies on her body and skills as a professional dancer to do her job.”
According to Carolyn, there was little to do immediately except quickly deal with the injury and continue her job as director and choreographer of the production. “I went to my local emergency department, got everything stabilized, got the pain managed and went back to the theater where I still produced the event that was so important to me,” said Carolyn. “On Monday, through networking and referrals, I was sent to St. Elizabeth’s Medical Center to see Dr. Hans Van Lancker, who was known as a surgeon for the Boston Ballet. I was really scared about surgery in general, but Dr. Van Lancker was so good at explaining everything to me, helping me be calmer. He fully shared my desire to return to dancing, and his confidence gave me the courage for surgery.”
“Carolyn’s injury was more than a simple ankle sprain. During the fall, she suffered an ankle fracture-dislocation and ruptured several ligaments,” explained Dr. Van Lancker. “She made it clear to me she wanted to dance again, and I reassured her my team would get her back in pointe shoes.”
The next day Carolyn was in surgery and knew she was entering the next phase of recovery. “I wanted to dance by the spring,” said Carolyn. “Dr. Van Lancker was fully supportive of that goal.”
The first week after surgery was challenging as Carolyn was immobile, but after that, she was able to focus on little goals like getting the boot off and sleeping more comfortably, moving her foot around and more. During this time, Carolyn kept busy with her radio show and her stand-up comedy along with teaching dance class on crutches.
As an athlete, Carolyn worked on her recovery with a regiment of Therabands, Pilates and stretches which, after the boot was able to be removed began swimming as well. Dr. Van Lancker approved an ankle brace that allowed her to use the stationary bike along with squats. She was using her kitchen counter as a ballet bar and doing exercises every day. After ten weeks Carolyn tried dancing again. And, while it didn’t feel the same as before, she was able to perform. “Sometimes I jump, and the landing feels a little rough, but I was able to go back en pointe in May 2018,” she said.
From here, Carolyn continued from strength to strength. “Healing is never linear. I felt I hit walls, but I always saw some progress and took courage from that. I had to listen to my body.” She was able to hike the Red Rocks in Sedona and also faced off against the ice at the Ice Castles in New Hampshire.
Key to it all was the support she received from her physician. “Dr. Van Lancker was on the same page as me. He helped me maintain my confidence and find little goals. I felt that Dr. Van Lancker was a little bit of a risk-taker like me, and he really listened and was able to try to support my goal of dancing again,” said Carolyn.
Minimally Invasive Hand Surgery Gives Guitar Player Back His Chords
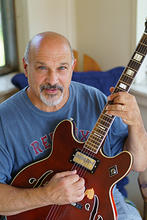
Gregory “Greg” S. started playing the guitar when he was 10 years old. When severe carpal tunnel syndrome began to significantly impair his playing, he knew it was time to pay attention to his symptoms.
“My fingers had forgotten how to play a “C” chord,” explained Greg. “They wouldn’t go where I told them to on the fretboard. I felt tingling from the tip of my fingers to the base of my knuckles and couldn’t even feel the tips of my fingers.”
For the better part of two years, Greg had been playing the guitar with symptoms. His hand would fall asleep while he was playing. “I had to shake my hand to resume playing,” said Greg. He was using a wrist splint at night and applying lotion throughout the day to manage the constant itching. Despite his symptoms, Greg continued his weekly hand stretches and flexibility exercises.
When it came time for his annual physical with his PCP, Dr. Paul Fallon, a member of Steward Medical Group, Greg decided it was time to tell him about the pain and symptoms in his hand. “At this point, I had “claw hand” at night,” said Greg. “Dr. Fallon has been my PCP forever. He immediately referred me to an orthopedic hand surgeon.”
Shortly after, Greg met with the medical team at the Boston Orthopedic Hand Center at St. Elizabeth’s Medical Center. The team specializes in hand and wrist surgery and treatment of carpal tunnel syndrome using a minimally invasive endoscopic technique.
A nerve test was performed by a neurologist and it confirmed what they suspected.
“Carpal tunnel syndrome is a condition where the major nerve going into your hand is severely compressed. When any part of your body is being squeezed, it is actually losing blood flow. And when you lose blood flow to the major nerve in your hand, the nerve is no longer getting the oxygen that it needs to function. In other words, the nerve itself is slowly dying. The damage to the nerve is reversible initially, but it can become irreversible once the nerve has lost too much oxygenation over time,” was explained to Greg, who was diagnosed with an extreme late-stage case. Had he waited longer, the long-term nerve damage could have been permanent. Fortunately, he was still a candidate for the minimally invasive endoscopic technique. Greg’s right hand was also showing the effects of carpal tunnel syndrome, though still within the normal range.
“From my first appointment with the center's team, I felt really involved,” said Greg. “I’m an engineer by trade, so I ask a lot of questions. I like to understand how things work. They always took the time to explain things in a way that I could understand and relate.”
Greg decided to move forward with hand surgery. “Before, during and after the procedure, everyone explained what they were going to do. They involved me every step of that way,” said Greg. While the endoscopic carpal tunnel release technique is done in an operating room, the patient goes home the same day. The minimally invasive technique requires only a small incision in the palm or the wrist.
For Greg, the relief was instant. “Immediately after the procedure my fingers were warm, the tingling sensation was gone, and I could feel my fingertips.”
After surgery, Greg had four sessions of occupational therapy with St. Elizabeth’s Rehabilitation and Physical Therapy Services. “At my first appointment, I could only lift 35 to 40 pounds. By my fourth visit I was lifting 80 pounds,” said Greg. He still does his exercises every day and can touch his thumb to his pinky without having to push them together.
“I feel like I have a brand new hand,” said Greg. “I had the surgery on a Tuesday, and by Thursday I was able to play the guitar. I’ve been playing every day since then. It’s amazing that a 30-minute procedure and a small incision can change things so significantly.”
Greg plans on having surgery on his right hand in the coming months. “If you’re affected by carpal tunnel syndrome and even considering surgery, talk to your PCP and call the team at the Boston Orthopedic Hand Center.”
For more information, contact the Boston Orthopedic Hand Center at St. Elizabeth's at 617-779-6500.
Jazz Singer, Psychologist Upstages Lung Cancer

Hildy G. is a psychologist by day and a jazz singer with Follen Angels by night. It was the fall of 2006 and she was in the middle of making a CD and enjoying the season.
“I was headed down my basement stairs in a new pair of green sandals with a cute heel when my feet went out from under me, like slipping on ice. One foot went back and the other scraped the wall in front of me. Fortunately, I was able to catch myself,” said Hildy.
The fall left Hildy with discomfort in her left wrist, elbow and right ankle so she decided to get checked out. She didn’t realize that this random accident would lead to an unexpected diagnosis. Hildy eventually had an MRI to see if she had pinched a nerve in her back. That wasn’t the case.
“The MRI picked up two tiny spots in my right lung,” explained Hildy. “My internist sent me for further tests and an eventual biopsy. The diagnosis was lung cancer.”
Hildy was referred to Dr. John Wain, a renowned thoracic surgeon. “The diagnosis and uncertainty was all very scary. I didn’t know anything about lung cancer,” said Hildy. “From the first time I met Dr. Wain I knew he would always have my back. I appreciated that he was very realistic and factual.”
Her surgery was scheduled for three weeks later. “I was able to remove the two small tumors in two lobes and a small section of tissue around the sites. The tumors were small and they hadn’t spread,” said Dr. Wain. “Because of her fall, her cancer was diagnosed early, stage 1A.”
It was after the surgery and finishing her CD that Hildy understood the gravitas of the bullet she missed, “Only 15 percent of people diagnosed with lung cancer have a 5-year survival rate. It’s the number one cancer killer for women.”
While recovering, Hildy read “The Alchemist” by Brazilian author Paulo Coelho. “It’s a book about learning to read the omens strewn along life’s path, and, above all, following our dreams. This wise guide said it was in my hands to make something of my experience,” reflected Hildy. “It spurred me to think about how I could make something worthwhile and life affirming out of having had lung cancer.”
Since Hildy’s surgery, Dr. Wain has joined St. Elizabeth’s Medical Center as the Division Chief of Thoracic Surgery and Vice Chairman of the Department of Surgery and Hildy started a non-profit, Upstage Lung Cancer, to raise awareness about lung cancer and raise money for cancer research.
Hildy followed Dr. Wain to St. Elizabeth’s.
“Dr. Wain is exactly the kind of doctor you dream about having. I trust him 100 percent and really appreciate his approach,” said Hildy. “He is always respectful and kind, extremely steady, really smart and always collaborative. When I have a scan he always reviews it step by step, discussing the similarities and differences.”
Dr. Wain and the thoracic surgeons at St. Elizabeth’s are using robotic-assisted surgery and minimally invasive video-assisted thoracic surgery (VATS) to treat lung cancer, and other lung related conditions.
Hildy encourages everyone to be aware of the risks and symptoms for lung cancer, know your family history and raise the topic with your PCP. Most importantly, she says to always advocate for yourself.
“The fact that I have had lung cancer is ever-present for me. My annual CT scans are wonderfully reassuring yet terrifying to anticipate. There is always that ‘What if’ feeling of fear,” said Hildy. Instead, she continues to turn her energy towards Upstage Lung Cancer. “My life has been about helping people and now I’m using my love for music and entertainment to fight lung cancer.”
Facing Thymoma with Dr. John Wain and the St. Elizabeth's Team

For Larry from Everett, Massachusetts, the stress and worry associated with a possible lung cancer diagnosis was like nothing else he ever faced in his life.
Larry first learned of a possible concern when doctors found a mass on his thymus, a small organ located beneath the breastbone that is included in the lymphatic system. This mass, or thymoma, would be part of his life until late 2017.
“I had an x-ray where they found the mass and then immediately the thought of cancer comes up and won’t go away,” said Larry.
After receiving a 2nd opinion after an MRI, he was told the mass had grown, was likely cancerous and needed to be removed immediately. Given the magnitude of the procedure, Larry checked around some more and found John Wain, MD, chief of Thoracic Surgery at St. Elizabeth’s Medical Center.
With his wife and sister by his side, Larry made an appointment with Dr. Wain which changed the course of his treatment.
“Before meeting Dr. Wain, I was initially recommended for robotic surgery at another hospital which sounded great as open surgery would require my sternum to be cracked,” said Larry.
However, after meeting Dr. Wain, Larry learned that this wasn’t his recommended course of action.
“While I was nervous at this point, I had heard nothing but good things about Dr. Wain,” said Larry. “He was a bit late for our appointment as he was in with another patient and I soon learned why. He was thorough, patient and really explained the situation to us. We never felt rushed and we asked him a ton of questions.”
According to Dr. Wain, Larry likely didn’t have cancer, “Larry was understandably nervous and concerned as his diagnosis seemed to be changing. After reviewing his imaging and his history, I felt that the mass, while unlikely cancerous, did need to be removed. And, given its location and size, a robotic procedure had a probability of leaving some of the mass behind which is dangerous. The only way I could help is through an open procedure. Larry’s health was good and his attitude was great and I felt that he would do well with the procedure.”
Larry was scheduled for surgery in November 2017 and, after the procedure was grateful for the prognosis. The mass did have a protrusion that would have been difficult to remove robotically as it might have broken during removal and left a lot of particles behind which would have then required radiation. However, Dr. Wain was able to remove the entire mass and, Larry was able to focus on recovery.
“I thought recovery was going to be long and painful. But after 3 or 4 days in the hospital I felt okay and went home shortly after.” said Larry. “I did remarkably well and feel great. I went back to work at my autobody shop in Everett. Through it all, Dr. Wain was always available, accessible and a source of calm reassurance.”
Larry’s future looks very positive. According to Dr. Wain, there is always a chance that future cancer could occur. However, regular CT scans will help the medical team keep on top of any future issues. “Larry has a great prognosis. I’m very pleased with his outcomes and delighted to have been part of his care team.”
For more information, visit St. Elizabeth’s Thoracic Surgery Department at https://www.semc.org/services-directory/thoracic-surgery or call 617-779-6382.
Marlena H. − A Patient’s Painting of Gratitude

For patients and visitors walking into the St. Elizabeth’s Medical Center St. Margaret’s lobby, they are greeted not only by a friendly face at the front desk but by a beautiful, custom made painting of a mother and two children. This painting is a special welcome to moms and dads and embodies our staff’s hopes and well-wishes for new and growing families.
The painting is a gift from St. Elizabeth’s patient Marlena H. from Brighton, Massachusetts, who is an artist and also mom to Ewa, or Eve, age 1 and Phoebe, age 5.
According to Marlena, the painting represents the concept of motherhood and was inspired by her own positive pregnancy with Ewa and labor and delivery experiences at St. Elizabeth’s.
“Do not be fooled by big shiny lobbies and fancy maternity rooms in big hospitals. Let the doctors and nurses shine instead,” Marlena recommended. “I know this hospital is a small one, but because of that, I feel like the patients can have a better relationship with a doctor. If you do not want to be rushed and if you want to be listened to then this is a great place for you to have your baby.”
Marlena’s relationship with St. Elizabeth’s began after becoming pregnant with Ewa in 2016.
“Due to the many complications I had while pregnant with Ewa, I needed weekly visits to the hospital. Because of this, I had a chance to get to know people who work at the St. Elizabeth’s OB-GYN department, including the doctors, nurses, billing, and front desk,” said Marlena. “Many people gave me extra time, helped me with scheduling multiple doctor’s appointments on the same days, and helped me with the billing department. The people who work at St. Elizabeth’s helped me more than they had to on so many different levels. My painting is there to remind them how thankful I am for them being in my family's life.”
Marlena’s first pregnancy with Phoebe was a challenging experience. Her OB-GYN, who was affiliated with a different Boston-based hospital, mistakenly scheduled her for a C-section four days before her due date.
“That scared me and my husband William, and made me feel very disappointed in my former OB-GYN,” said Marlena. “I ended up with an emergency C-section two weeks later that left very painful scars for five years. I could not lift my arms up without very sharp pain. Since that time, I was truly a broken person; physically and mentally. For my second pregnancy, I decided to try a smaller hospital. I'm very glad I did because I'm a ‘healed’ person today.”
According to Marlena, St. Elizabeth’s is within walking distance of her home in Brighton. She was able to walk to the hospital for her appointment with her midwife, however, early in the pregnancy, Marlena began to experience complications, including gestational diabetes, anemia, was placed on a miscarriage watch and categorized as a high-risk pregnancy. At this point, obstetrician Jean Noel, MD, was called in to assist.
“I think during the second or third month I asked Dr. Noel what were the chances that the baby will survive,” explained Marlena. “He said about 50 percent. It was stressful.”
Marlena felt that with Dr. Noel and Erin Gonzalez, NP, she received time and attention, felt comfortable asking questions, and did not feel rushed.
“Pregnancy is an incredibly important time in a women’s life,” said Dr. Noel. “We associate this time with positive feelings, but for many women like Marlena, there are complications and, frankly, scary situations that require more intensive medical involvement. As a doctor, it is important to care for each mom as an individual and make sure that they are in a situation where they are receiving the best health care available. I was very happy for Marlena when she delivered beautiful Ewa.”
For Ewa’s birth, Marlena recalls being incredibly anxious. After careful follow up with Dr. Noel, Marlena was hospitalized a few days before Ewa’s birth. And, despite her fears, she said that Ewa’s birth was a magical experience.
“The room was full of people helping me,” said Marlena. “When Ewa was born, I held her immediately. I did not experience that with Phoebe. That was a day and night experience.”
And for her follow-up, Marlena felt a deepening gratitude toward the people who were involved in her pregnancy and labor and delivery care.
“I remember bringing my first daughter, Phoebe, with me to a follow-up appointment with our previous doctor. While she was happy to see Phoebe, her reaction was nothing link Dr. Noel’s,” Marlena recalled. “He asked me if he could hold her. He held her and rocked her. Those little things make a huge difference in mother’s life!”

With two active girls at home and a first-time kindergartner along with maintaining her art career, Marlena is busy these days. After Ewa’s birth, Marlena received a commission to work on a painting for a mom in Texas who was expecting twins. While working on this commission, she was able to channel some creative energy into the art she donated to St. Elizabeth’s. “I'm very honored that the hospital accepted the painting and that you find such a special place to share it with the public,” said Marlena.
And the public appreciates it. According to Margi Leffer, who works in administration in the Department of Obstetrics and Gynecology, "So many people tell me how much they love this painting. I love seeing it each morning when I come to work.”
“Some people go to work to make a living every day, and then there are some people who live to make a difference through their work...every day,” said Marlena. “Thank you, St. Elizabeth's OB-GYN team!”
For more information about Marlena and her work, visit her website at http://www.marlenabocian.com/. For more information about OB-GYN options at St. Elizabeth’s, visit the Steward DoctorFinder™.
Brenda T.
In 2014 my husband had open heart surgery at St. Elizabeth’s Medical Center in Brighton. This was a very difficult time for our family. My family and I were truly grateful for the dedication and expertise level of care my husband received. But, what was especially significant during this stressful time and for which we were most grateful was having the Bikur Cholim room at the hospital.
The special Bikur Cholim room at St. Elizabeth’s provided us with a lovely rest area, kosher food at the highest level and a quiet place for prayer.
We appreciated having such a place available to us and we thank St. Elizabeth’s for their kindness and compassion in meeting a real need for observant family members.
Brenda T., Brookline, Massachusetts
Carl M.
Before retiring to spend half the year in Florida, Carl M., who goes by Mitch, of North Attleboro first had to do something about progressively worsening Atrial Fibrillation (AF). He was taking five or six arrhythmia drugs daily and suffered from chronic sluggishness and sleepiness. He had reached a point in which he would come home from his demanding job every day and take a nap, a behavior his wife became increasingly concerned about.
AF is an abnormal rhythm of the upper chambers of the heart causing electrical impulses traveling to the bottom part of the heart to create an irregular and/or fast heart rhythm. Symptoms can include:
- Fatigue
- Palpitations
- Shortness of breath
- Chest discomfort
- Dizziness
- Swelling in the legs
- Fluid accumulation in the lungs
For Mitch, his AF was actively managed for several years. He was prescribed various medications, which he took until they no longer worked, and had two cardiac ablations each of which helped his symptoms for about a year-and-a-half-to-two years each time.
Then, in April 2016, after being evaluated for a third cardiac ablation, his cardiologist Dr. Waqar Cheema in Wrentham, Massachusetts referred him to St. Elizabeth’s cardiac electrophysiologist John Wylie, MD, FACC and cardiac surgeon Stanley Tam, MD, FACS, FACC to discuss a new procedure they were offering for patients with difficult-to-treat AF. The procedure, known as the Convergent Procedure, is a revolutionary treatment for patients with difficult-to-treat AF in which a cardiac surgeon and an electrophysiologist work together for a more permanent solution to manage persistent AF.
“Dr. Cheema told me it was time to go see the boys in Boston,” said Mitch. “The medication no longer worked and a third ablation didn’t look promising for long-term results. Dr. Cheema knew of a relatively new procedure that he felt I was a perfect candidate for.”
According to Dr. Wylie, the Convergent Approach is a powerful option for many people in whom AF is difficult to control. The procedure starts with a cardiac surgeon first performing a minimally invasive laparoscopic ablation across the back wall of the heart via a small incision in the abdomen. Then the next day, a cardiac electrophysiologist completes the procedure and checks for other arrhythmias by threading an ablation catheter through a patient’s femoral vein in the groin to the inside of the heart. Radio wave energy is sent through the tip of the catheter to create scar tissue at specific areas of the atrium where AF originates and completes a thorough ablation set in the heart. Electrophysiology diagnostics are then used to confirm the abnormal electrical signals were interrupted and that no other arrhythmias remain that need to be treated. Most patients treated with the Convergent Approach are able to go home within two to four days, resume a more active lifestyle, and may be able to stop taking medication to treat AF.
“Dr. Tam and Dr. Wylie were very thorough,” said Mitch. “Even my wife, who was nervous on my behalf, felt confident after we reviewed the procedure.”
Mitch spent a total of four days in the hospital and, besides the recovery from anesthesia, he stated he had no pain and, if not for the bandage, wouldn’t have known he even had the procedure. “I can’t believe how good I felt,” said Mitch. “I was pain free and started to feel my sluggishness and sleepiness quickly fade. When I walked my knees and back would hurt and now they don’t. I think I have better blood flow and just overall feel better.”
Mitch said the team of Dr. Wylie and Dr. Tam made appointments easy to schedule, worked collaboratively and generally took good care of him. He recalls, “one of the things I remember is that the procedure was scheduled for July 5, 2016. On the afternoon of July 4th, Dr. Tam called me at home to make sure I was feeling okay, answer any questions I had and generally reassure me before the next morning. I cannot speak highly enough of all of them; Dr. Cheema, Dr. Tam and Dr. Wylie.”
“This is the best I have felt in five year,” said Mitch. “I don’t know how bad I was feeling until after the Convergent procedure.”
Now, while enjoying retirement, Mitch is spending time with this wife, looking forward to meeting a new granddaughter who was born this past winter and walking to help address additional weight loss that he wants to achieve. “I’m hoping that I can lose enough weight that I no longer need the blood pressure medication,” said Mitch. “And, I’m hoping that at my check-up with Dr. Wylie in April 2017, I can also stop taking the blood thinner.”
Angelo C.
At 87 years old, Angelo C. likes to stay on the go. The Winthrop, Massachusetts resident attends church every day, goes to the mall and grocery store once a week, and likes to hang out downtown. His motorized wheelchair and heart condition don’t slow him down.
Angelo, who has congestive heart failure, regularly sees Cardiologist Dr. Joseph Carrozza at St. Elizabeth’s Medical Center. As part of his treatment plan, Angelo is benefiting from the state-of-the-art CardioMEMS™ System, which features a miniature wireless monitoring system that is implanted in the pulmonary artery during a minimally invasive procedure to directly measure pulmonary artery pressure. What make this system unique is it allows Angelo to transmit pulmonary artery pressure data from his home to his health care team allowing for personalized and proactive management to reduce the likelihood of hospitalization so he can continue to enjoy his lively lifestyle.
“Angelo was a perfect candidate for CardioMEMs,” says Dr. Carrozza. “I explained to him that the greatest benefit of having the implanted monitoring system is that it will keep him out of the hospital.”
On March 20, 2016, Dr. Carrozza performed the hour-long, painless procedure to insert the monitoring system using a catheter into Angelo’s pulmonary artery. He was awake throughout the whole procedure and following the procedure, he had to stay still, without moving, for six hours. During this recovery period, the cardiac catheterization lab nursing staff cared for him.
“The nursing staff was fantastic and went above and beyond to help me,” says Angelo.
“I use The Ride to get back and forth to St. Elizabeth’s. When the driver arrived to take me home after the procedure, my six hours wasn’t up and they left. I had no way to get home. One of the nurses said ‘I’m going to take care of you.’ She arranged for an ambulance to take me home, as well as confirmed my insurance would cover the transport. She and another nurse stayed well after their shifts ended to make sure I was taken care of and got me into the ambulance. They didn’t go home until I got home.”
Nowadays, back at home in the early afternoon, Angelo takes a break from his daily activities to hook himself up to the CardioMEMS™ System for his reading. His fastest reading was three seconds, and the longest was 15 seconds. He feels the time it takes for a reading all depends on the positioning of his body.
“It is amazing that I am here, at my home, and my doctor, in Boston, can receive my exam and know if I am okay or if I need something, like an adjustment in my medicine,” says Angelo. “This is such a benefit to me, the patient. It is like having a doctor in my house everyday giving me an exam. What more could you want?”
Debbie A.
When routine care turns into specialized care.
More than 52 years ago, Debbie A., of Arlington, Massachusetts, delivered all three of her children at St. Elizabeth’s Medical Center and has been receiving routine care at the hospital ever since. Recently, this routine care changed for the 75 year old after she was diagnosed with reoccurring breast cancer.
In November 2014, Debbie had a screening mammogram at St. Elizabeth’s Center for Breast Care and it showed a lesion on her left breast. Then, a biopsy confirmed cancer. Working with Jan Rothschild, MD, a breast surgeon at St. Elizabeth’s, Debbie had a mastectomy on her left breast in December. She had already had a mastectomy on her right breast when cancer was detected in 1989.
"I am the sole caregiver for my 47-year-old daughter who has multiple sclerosis and was diagnosed as a teenager,” says Debbie. “I’ll do anything to be here for my children and I knew when I first met Dr. Rothschild, whose smile beamed right through me, that I wanted her to be my doctor through this journey.”
Debbie’s recovery went well and she takes anastrozole, a chemotherapy medication, for further treatment. In addition to the care she received from Dr. Rothschild and her medical oncologist, Leslie Martin, MD, Debbie was also overseen by a nurse navigator who was her guide, mentor and advocate before, during, and after her treatment.
“All of the staff at the Center for Breast Care was wonderful and my nurse navigator, Cheryl, was unbelievable,” explains Debbie. “From day one, she made me feel that everything was going to okay. Knowing this made me feel good and confident.”
Manuel G.
For the past 50 years, engineer Manuel G. has routinely worked seven days a week and played racquetball and competitive soccer. About 18 months ago he began needing naps to get through the day, doubling over to catch his breath while playing sports and experiencing heart palpitations.
“I felt like an old man. I didn’t have any energy,” Manuel, 71, of North Dartmouth, Massachusetts, said.
In May of 2014, he was diagnosed with persistent atrial fibrillation, a condition where a patient has a sustained heart rhythm disorder for more than seven days. A procedure called a cardioversion got his heart beating normally again, but only for a few days. A second one lasted about a week. His cardiologist then reached out to Dr. Michael Orlov, director of the Electrophysiology Laboratory at St. Elizabeth’s Medical Center. He underwent a third procedure called an ablation where Dr. Orlov used radiofrequency to produce scar tissue on Manuel’s heart to block abnormal electrical signals that cause his rhythm disorder. In less than two weeks he was back in atrial fibrillation and by the end of the year he had undergone a second cardioversion and another ablation, however, in his case, they did not correct his condition.
“I really, really, didn’t want a pacemaker,” he said. “That was out of the question for me.”
On the advice of Dr. Orlov, Manuel met Dr. Stanley Tam, a cardiac surgeon who had recently joined St. Elizabeth’s Medical Center from the University of Massachusetts Memorial in Worcester where he had served as chief of cardiac surgery. After consulting with Dr. Tam and Dr. Orlov, Manuel decided to undergo an ablation procedure called the “Convergent Approach” where the cardiac surgeon and electrophysiologist work as a team to perform a cardiac ablation. Using a minimally invasive approach with a small incision in Manuel’s abdomen, Dr. Tam performed an ablation across the backside of his heart. Dr. Orlov, the next day, threaded an ablation catheter through Manuel’s femoral vein in the groin to reach the inside of his heart to ensure the lesions were completed and connected, and then used electrophysiology diagnostics to confirm the abnormal electrical signals were interrupted.
“I’ve been in normal sinus rhythm since,” Manuel said. “I’m feeling the best I have felt in two years.”
Manuel, who has been married for 50 years and is a father and grandfather, is doing just that. In the summer heat and humidity, he was building a patio at his house and is once again playing racquetball.
“I’m really thankful to my doctors for giving me back my life,” he said.
Lucy M.
Last year, when Lucy M. began experiencing problems with her breathing, she chalked it up to complications stemming from her asthma. She followed up with her pulmonologist who adjusted her medications. When the breathing problems persisted, she consulted with her primary care physician who referred her to a cardiologist. A heart catheterization revealed a narrowed heart valve, a condition called aortic stenosis.
In June of 2015, Lucy, 84, underwent a transcatheter aortic valve replacement (TAVR) at St. Elizabeth’s Medical Center. The procedure is one in which the technology allows physicians to replace a severely narrowed aortic valve due to aortic stenosis without a conventional chest incision or having to be placed on a bypass pump. In this much less invasive approach, a new valve is implanted either through a catheter that is inserted through the vein in the groin area and then carefully passed up into the heart, or through a tiny incision in the chest wall and implanted directly into a patient’s heart.
“I feel good, really good,” Lucy, of Haverhill, Massachusetts says. “I’m surprised I feel as well as I do.” Without the TAVR, she faced an uncertain future and is pleased she underwent the procedure.
“I’m 84 years old. I felt either it’s going to do good for me or it’s not going to do good for me, so I thought I would take the chance,” she says. “I want to prolong my life. I still feel young.”
She encourages others who need this procedure to give it a try. While she misses working, she doesn’t miss her commute. Faced with several other health issues, Lucy is content to spend time with her adult son and daughter and do “ordinary things,” including grocery shopping, laundry and cooking.
“If anyone has the opportunity, regardless of what age they are, they should take the chance. Always take a chance,” she says.
